How much chocolate cake do you want to eat?
It depends on what your hormones are telling your brain. Hunger and satiety may seem like straightforward sensations: You feel hungry when you need to eat and then you feel full after you’ve consumed enough. But the reality is more complicated. A group of hormones works together behind the scenes to control hunger, fullness, and fat storage, impacting your body weight and overall health.
Here’s a closer look at seven of the major players in appetite regulation.
Leptin
Scientists used to believe that fat in our bodies was just a storage place for extra energy. But now, we know that fat is more complex. It actually behaves like an organ, producing hormones, one of them being leptin.
When we eat, our fat cells release leptin to signal to our brain that we've had enough food, so we don't overeat.
If someone is overweight, they usually have higher levels of leptin because they have more fat in their body. However, sometimes their body becomes resistant to the effects of leptin, which means the brain doesn't respond properly to the signal to stop eating.
On the other hand, if someone cuts down on the number of calories they eat and starts losing fat, their leptin levels go down. This happens because leptin tries to protect the body from losing too much fat, and it's related to the body's natural weight control system.
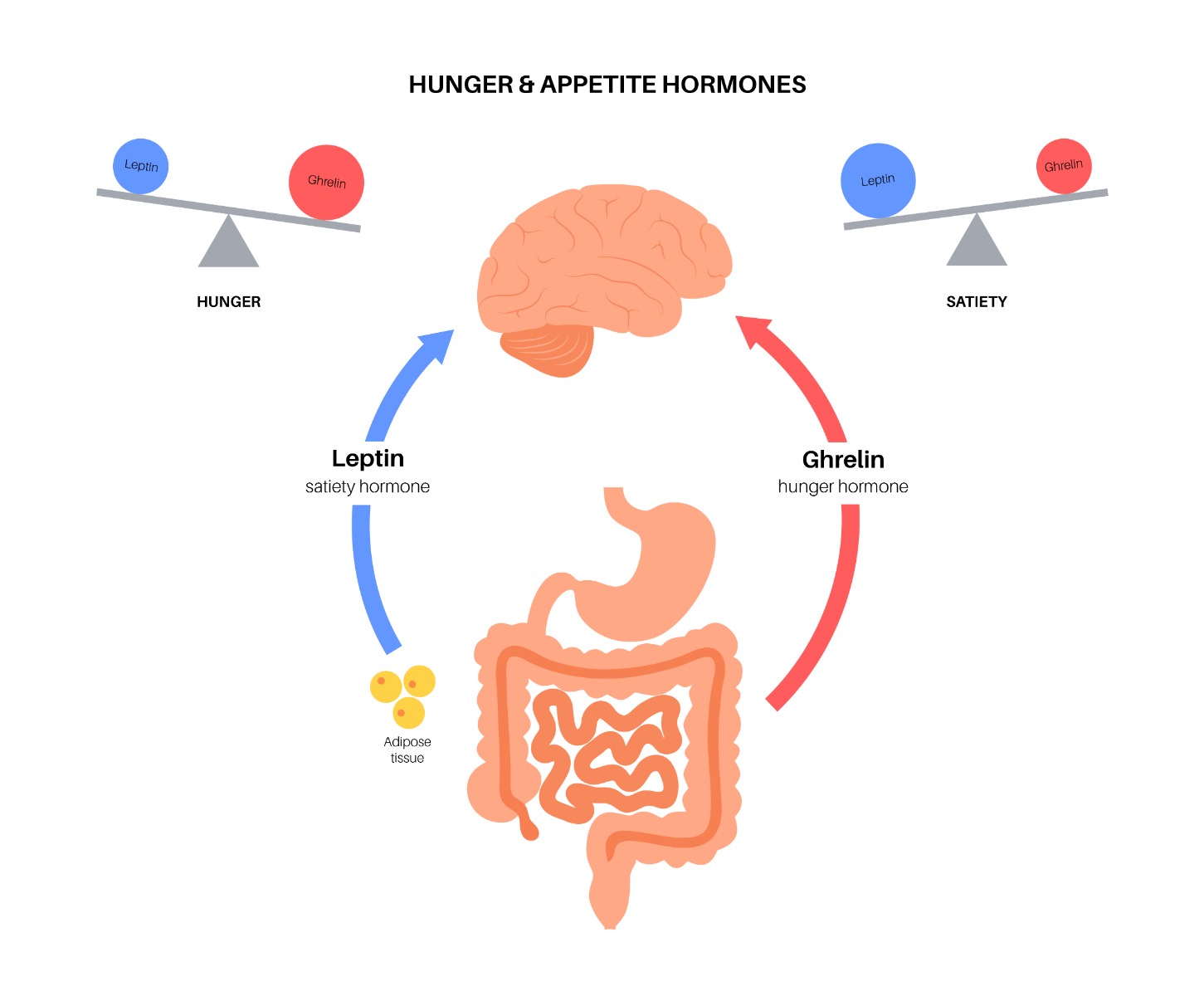 Ghrelin
Ghrelin
Often called the “hunger hormone,” ghrelin is produced by the stomach. Before you eat, ghrelin levels are high, but they decrease after a meal. When you try to lose weight by cutting calories, your ghrelin levels actually increase from their usual baseline. This increase in ghrelin makes you feel hungrier than usual, which can make it harder to stick to your weight loss plan.
Researchers have found that people with higher baseline levels of ghrelin tend to have stronger food cravings, especially for high-fat or sweet foods. Additionally, these individuals may experience greater weight gain over time, making it challenging for them to achieve their weight loss goals. Understanding its effects can help us find better ways to manage our weight and make healthier food choices.
Insulin
Insulin is a hormone made by the pancreas, and it helps regulate the amount of sugar (glucose) in your blood. When you eat foods with carbohydrates, your blood sugar levels go up, and in response, the pancreas releases insulin. Insulin's job is to take the excess sugar from your blood and move it into your cells to use as energy.
However, sometimes the body doesn't respond well to insulin, and this is called insulin resistance. It can be related to certain lifestyle factors such as being overweight, not physically active, or eating a lot of sugary foods and simple carbohydrates.
Cortisol
Cortisol is a hormone often linked to stress because our bodies produce more of it when we feel stressed. But cortisol does more than just respond to stress—it also helps regulate our metabolism. When cortisol levels are higher than their usual baseline, it can lead to insulin resistance, which means our bodies have trouble processing sugar and may store more fat.
When we experience chronic stress, our cortisol levels can surge, making us feel more hungry, especially for sweet, salty, or fatty foods. This can cause our blood sugar and insulin levels to go up as well. A recent study showed that higher cortisol levels can increase our appetite and also reduce blood flow in certain brain regions that control our food intake.
Cholecystokinin (CCK)
After you eat, your gut produces a hormone called CCK, often referred to as the "satiety hormone." CCK helps you feel full and satisfied after a meal. It also helps with digestion by slowing down the movement of food from the stomach, which makes you feel fuller for longer. Additionally, CCK encourages the release of fluids and enzymes from the pancreas to help break down fats, proteins, and carbohydrates in food. The exact way CCK functions is not fully understood yet.
Glucagon-like peptide-1 (GLP-1, for short)
After you eat, a hormone called GLP-1 is released in your gut. It talks to your brain, making you feel full and satisfied. Also, it slows down digestion, keeping food in your stomach longer, which means you feel full for a more extended period.
Glucose-dependent insulinotropic polypeptide (GIP)
After you eat, the small intestine produces a hormone that boosts insulin levels. This increase in insulin stimulates the production of glycogen and fatty acids, which prevent the breakdown of fat. This hormone, known as GIP, is relatively new, so there's still much we don't know about it.
What is the role of genes in regulating hunger hormones?
Genes play a role in how our bodies react to food and how hormones like leptin and ghrelin function. Certain genes, like MC4R, ESR1, and FTO, can impact your eating habits by regulating these hormones. Read to find out more about these genes: https://mapmygenome.in/blog/the-genetics-behind-eating
How does MyFitGene™ helps in understanding your eating behaviour?
MapmyGenome™’s MyFitGene™ is a DNA-based sports, fitness, and nutrition assessment test, which has been carefully designed to target 40+ hand-picked parameters that affect nutrition, fitness, and wellness of an individual.
This comprehensive test delves into your genetic makeup, providing valuable insights into genes that influence your fitness potential, dietary preferences, eating behavior, hunger muscle strength, heart health, vitamin levels, and more. By studying your unique genetic profile, MyFitGene™ offers a personalized and in-depth report, personalized to you.
Moreover, our expert genetic counselors are here to help you understand the genetic results and offer personalized recommendations.
Your genes, diet, and lifestyle all affect your eating habits. By knowing your genetic profile and modifying your diet and lifestyle, you can eat better.
And did we say it’s just a simple cheek swab!!!
References
Kiecolt-Glaser, Janice K., et al. “Omega-3 supplementation lowers inflammation and anxiety in medical students: a randomized controlled trial.” Brain, behavior, and immunity, vol. 25, no. 8, 2011, pp. 1725-1734. PMC, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3171260/
Gutiérrez, Salomé, et al. “Effects of Omega-3 Fatty Acids on Immune Cells.” International journal of molecular sciences, vol. 20, no. 20, 2019, p. 5028. MDPI AG, https://doi.org/10.3390/ijms20205028
Calder, Philip C. “Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology?” British journal of clinical pharmacology, vol. 75, no. 3, 2013, pp. 645-662. Nature Publishing Group, https://doi.org/10.1111/j.1365-2125.2012.04374.x.
Ramanathan, Sowmya and Das, Nandini P. “Omega-3 Fatty Acids.” StatPearls [Internet], StatPearls Publishing LLC., 2021 Jan-. NCBI Bookshelf, https://www.ncbi.nlm.nih.gov/books/NBK546653/
Dasarathy, Jaividhya and McCullough, Arthur J. “Sarcopenia and Cachexia in Chronic Liver Disease.” Clinics in liver disease (Hoboken), vol. 11, no. 1, 2018 Jan., pp. 24-27. NCBI Bookshelf, https://www.ncbi.nlm.nih.gov/books/NBK541120/