Alzheimer’s disease is a neurodegenerative condition resulting in progressive loss of memory and cognition.It is the most common form of dementia. For most people with Alzheimer's, symptoms first appear in their mid-60s or later this is referred to as the late onset Alzheimer’s disease. When the disease develops before age 65, it's considered early-onset Alzheimer's, which can begin as early as a person's 30s, although this is rare.
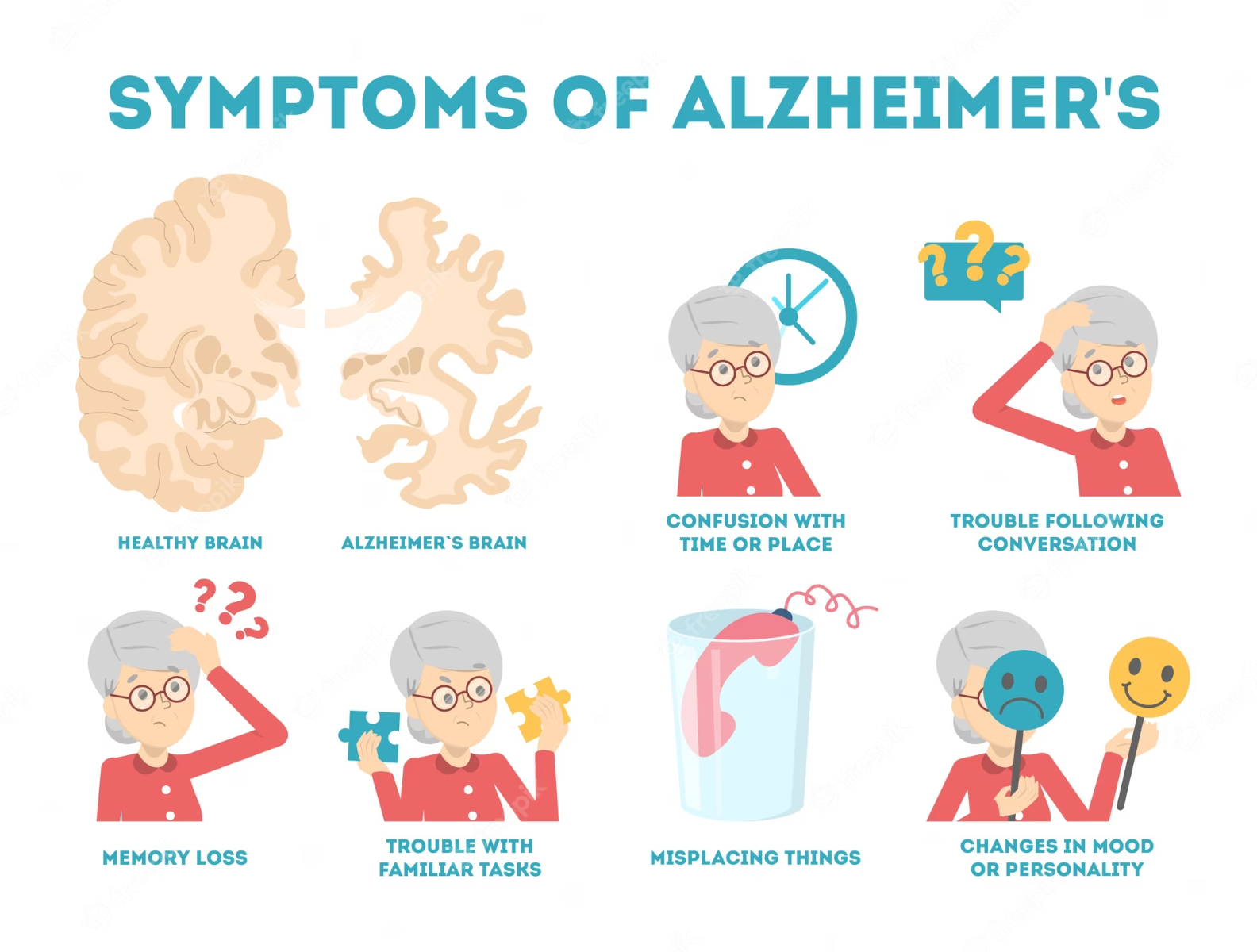
The early signs of Alzheimer's disease include:
- Memory loss that disrupts daily life, such as getting lost in a familiar place or repeating questions.
- Trouble handling money and paying bills.
- Difficulty completing familiar tasks at home, at work or at leisure.
- Decreased or poor judgment.
- Misplacing things and being unable to retrace steps to find them.
- Changes in mood, personality, or behavior.
Alzheimer’s is a progressive disease, the time from diagnosis to end-stage disease can be variable ranging from as little as three or four years if the person is older than 80 when diagnosed, to as long as 10 or more years if the person is younger. Initial symptoms can begin with difficulty in driving a car, and difficulty in paying bills. they may ask the same questions over and over, get lost easily, lose things or put them in odd places, and find even simple things confusing. As the disease progresses, some patients may present with emotional responses such as people becoming worried, angry, or violent.
Caring for individuals with Alzheimer’s disease
Caring for individuals with Alzheimer’s disease can be challenging, both physically and emotionally. Individuals and caregivers face different challenges in different phases of the disease.
In the early stages of the disease, most people function independently. They still drive, take part in social activities, volunteer and even work. A role of a caregiver is to provide support and companionship, and help plan for the future. With an early diagnosis, you and the person with dementia now have the opportunity to make decisions about the future together, including legal, financial, and long-term care planning.In India, with limited resources and long term support, families are often left isolated in caring for aging family members diagnosed with dementia. Some of the factors listed below can be helpful tips in organizing for care for family members:
- Safety first: Is there an immediate safety risk for the person with dementia to perform this task alone?
- Avoid stress: Prioritize tasks or actions that do not cause unnecessary stress for the person with dementia. For example, if you know that grocery shopping will be frustrating for the person with dementia, ask for their participation to outline a weekly menu and organize a grocery list.
- Make a positive assumption: Assume that the person with dementia is capable of completing the task. If you sense frustration, try to identify the cause of the frustration before intervening. For example, you use a phrase like, “Is there anything I can do to help?” or a nod to signal that it’s ok to chime in if the person with dementia is having difficulty remembering a word or name.
- Talk it over: The best way to determine how and when to provide support is to ask directly. Ask the person with dementia what they need or the frustrations they may be experiencing. Talk about it, then make a plan.
- Work better together: Find activities to do together and keep the conversation going about expectations for how you will provide support. Check in regularly by asking the person with dementia if you are providing a level of assistance that is comfortable or adequate.
The late stage of Alzheimer's disease may last from several weeks to several years. As the disease progresses, intensive, around-the-clock care is usually required. Individuals may need help with daily activities such as bathing, eating, using the toilet and may eventually need hospice care.
Ongoing treatments
Any treatment or clinical trials needs to be discussed and evaluated by your clinicians. Every person with dementia is different and would need different treatment approaches.
The FDA has approved medications that fall into two categories: drugs that change disease progression in people living with early Alzheimer's disease, and drugs that may temporarily mitigate some symptoms of Alzheimer's dementia. Drugs in this category slow disease progression such as anti-amyloid drugs They aim to slow the decline of memory and thinking, as well as function, in people living with Alzheimer's disease.These treatments change the course of the disease in a meaningful way for people in the early stages, giving them more time to participate in daily life and live independently. Clinical trial participants who received anti-amyloid treatments experienced reduction in cognitive decline observed through measures of cognition and function.
As Alzheimer’s progresses, brain cells die and connections among cells are lost, causing cognitive symptoms to worsen. While medications such as Cholinesterase inhibitor or glutamate regulators do not stop the damage Alzheimer’s causes to brain cells, they may help lessen or stabilize symptoms for a limited time by affecting certain chemicals involved in carrying messages among and between the brain's nerve cells.
Causes and risk factors of Alzheimer’s disease
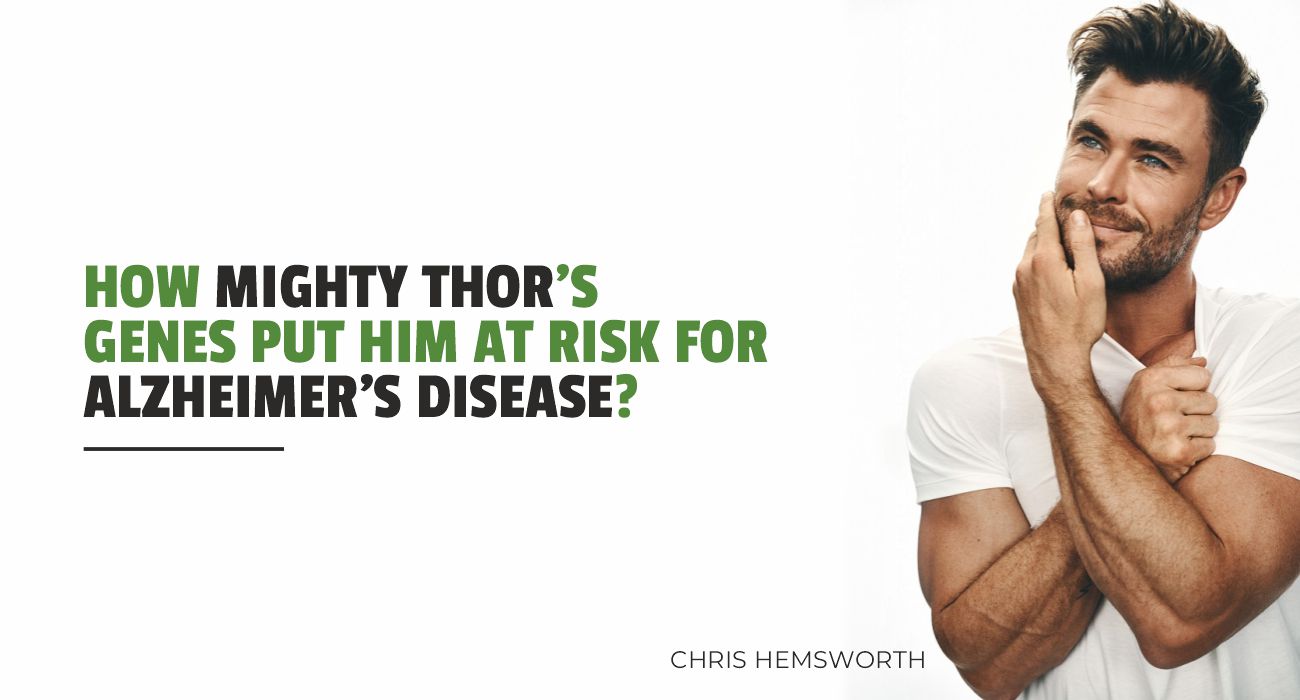
While certain genetic factors can increase risk of developing Alzheimer’s disease. There are many other non-genetic factors that increase risk as well. One genetic risk factor that has been identified to increase the risk for Late-Onset Alzheimer’s is the APOE e4 gene. However, inheriting one or two copies of APOE e4 does not guarantee that the individual will develop Alzheimer’s disease. It increases the risk of disease but it is not 100%.
About 5% of individuals diagnosed with Alzheimer’s disease are diagnosed prior to age 60. This is also known as Early Onset Alzheimer’s Disease. Of these, about 2-3% individuals are identified to have genetic mutations in genes such as APP, PSEN1 and PSEN2 which increases their risk of developing Alzheimer’s disease. Most individuals inheriting genetic changes in these genes develop Alzheimer’s disease by the age of 75 years.
Genetic counseling can help individuals understand the risks, benefits and limitations of testing. Genetic counselors can help anticipate what to expect from the test and facilitate informed decision-making regarding the test and its outcome.
Prevention is better than cure
While we cannot change genetic factors, we can alter our dietary and lifestyle factors that may be increasing the risk of dementia or Alzhemiers disease. Some of the non-genetic factors that we can alter include
- Oxidative stress which can damage nerve cells increasing antioxidants in our diet can be improve
- Continuously learning can improve neural reserve this protects your brain from early damages due to dementia
- Hypertension
- Type 2 diabetes
- Dietary factors: same factors that contribute to poor heart health also increase one’s risk of cognitive decline or developing Alzheimer’s disease. It is very important to eat in moderation and maintain a healthy body weight, as people who are obese double their risk of developing dementia according to the Alzheimer’s Association
MapmyGenome's Genomepatri™, a DNA-based health and wellness test that gives you a comprehensive assessment of your health helping you learn about your predisposition to conditions like Alzheimer’s Disease. Consulting a genetic counselor after taking these genetic tests can help you in understanding your health from a genetics standpoint. Mapmygenome’s genetic counselors consider your family history and guide you through the genomic report. They help you in interpreting the results, assess the implications of results, and create a personalized plan to prevent or delay the onset of Alzheimer’s Disease.