Congenital heart defects (CHD) are the most common form of birth defects affecting over 7 in 1,000 children worldwide. In Asia, the prevalence of CHD is about 9.3 per 1,000 births. A CHD doesn’t necessarily have to be life-threatening. Today, an increasing number of babies who are born with CHD are living healthy and longer lives. In fact, the vast majority (about 75-85%) of children born with CHD will live well into adulthood.
Congenital means something that is present at birth. Congenital heart defects refer to a group of heart defects that are present at birth. These defects may arise from issues related to the development of one or more parts of the heart during early fetal development. Babies born with CHD may appear healthy for the first few hours or days of life, after which they may present with signs or symptoms. Some of the common signs or symptoms that may be apparent are:
- Abnormal heart sound during a heartbeat (heart murmur)
- Rapid breathing
- Low blood pressure
- Low levels of oxygen
- Blue or purple tint to the skin due to lack of oxygen
Congenital heart defects may affect the normal functioning of the heart in different ways:
- Defects can increase pressure and stress on the lungs by re-circulating oxygenated blood to the lungs again. Some examples of such CHDs are Atrial Septal Defect, Ventricular Septal Defect, or Atrioventricular Canal.
- Redirecting un-oxygenated blood to our body. Babies with such defects may look blue due to lack of oxygen. Some CHDs that fall under this category include Tricuspid Atresia, Pulmonary Atresia, Tetralogy of Fallot, or Double Outlet Right Ventricle.
Many mothers will often wonder if they did something during the pregnancy to cause the heart defect. It is important to remember that most forms of congenital heart defect have no known cause. CHD is a complex condition with a variety of genetic and environmental (non-genetic) contributors.
Non-genetic risk factors
- Environmental teratogens or chemicals that can affect the growth of an embryo, for example, pesticides, dioxins, polychlorinated biphenyls.
- Maternal exposures to alcohol, thalidomide, anti-seizure medications, or infection such as rubella. It is important to note here that anti-seizure medications may be essential for the well-being of the mother and the fetus. If you are currently pregnant or planning a pregnancy and have the need to take anti-seizure medications, it is essential you discuss the risks, benefits, and safety of taking these medications during pregnancy with your doctor.
- Other emerging risk factors for CHD are obesity, diabetes, and high cholesterol.
Genetic contributors
Syndromic
Most cases of CHD are non-syndromic. This means that they are isolated and may occur in the absence of other health conditions or symptoms. However, in some cases, heart defects may occur as part of a genetic syndrome that may present with additional features including CHD. Some examples of such genetic syndromes include Down syndrome, Turner syndrome, and 22q11.2 deletion syndrome.
Single genes
Sometimes there may be a family history of CHD that could indicate an underlying genetic cause. Disease-causing changes in genes involved in the normal heart development before birth could cause CHD. There are single gene changes known to be associated with CHD.
Management
Many congenital heart defects can be picked up during a pregnancy at the time of routine ultrasound scan. Some may be picked during the 16-20-week ultrasound scan, while others may not be discovered until the baby is born. Sometimes, CHD may go undiagnosed until children are older and start to show symptoms. If there is a suspicion of a heart defect between 16-20-weeks of the pregnancy, you may be recommended to meet with a specialist. Follow-up exam using a fetal echocardiogram may be recommended.
Simple congenital heart defects may need minor or no management. In fact, some simple heart defects may be transient, correcting themselves as children grow older. On the other hand, some CHD may cause serious health issues that warrant treatment; some children may need surgery to correct the defect as soon as a few hours after birth. A pediatric cardiologist will monitor symptoms and manage health before and after correction of the defect. Despite high success rates of surgery, many children in India are not diagnosed in time due to lack of prenatal care, awareness, and funds.
Most children with CHD who receive appropriate treatments and/or interventions can lead a normal life. In some cases, exercise and other activities may be limited. Few children with CHD may have developmental delays or learning difficulties. Adults with CHD may need further treatment as they may experience complications at different times of their life. It is important for individuals with CHD to transition to appropriate cardiac care as adults and receive routine follow-up. Pregnancy is safe for most women with CHD. However, as a woman’s heart works harder during pregnancy and childbirth, it is important to monitor and manage pregnancy appropriately.
Precautions during pregnancy
Pregnancy is a unique time, along with the excitement of giving birth to new life, there is significant anticipation and anxiety surrounding pregnancy. Learning about a birth defect in your baby during pregnancy or after birth can be quiet distressing for the family. The cause for most CHD remains unknown. However, if you are pregnant or planning a pregnancy, you can reduce risk:
- Receive vaccination against Rubella
- Take folic acid supplements
- Speak with your doctor about medications during pregnancy, including herbal remedies and over the counter medicines
- Try to avoid exposure to chemicals such as dry-cleaning agents, paint thinners, and nail polish removers
- Avoid smoking and alcohol
- Maintain a healthy diet with good blood sugar control
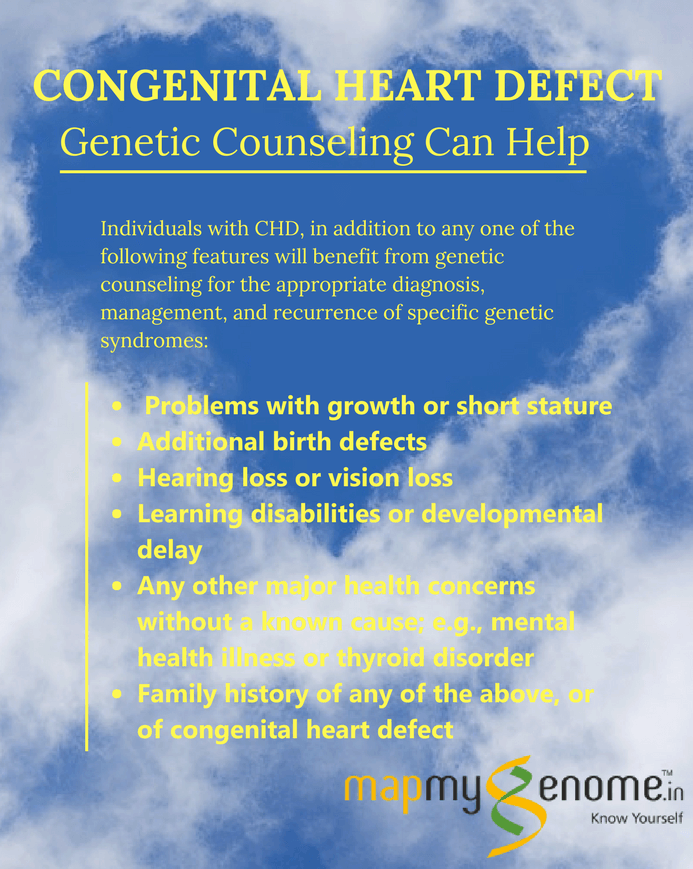
Living with CHD can result in significant physiological, emotional, and socioeconomic challenges for patients and their family. If you are an adult with a history of congenital heart defect or a parent of a child with CHD, speaking with a genetic counselor can help you to better understand the diagnosis and discuss emotional and medical implications for yourself and your family members. A genetic counselor is a specialized health care professional who has expertise in medical genetics and psychological counseling.
If you would like to set up a genetic counseling appointment CALL US on 1800 102 4595 (toll-free) or 040-66986700 or WRITE TO US at info@mapmygenome.in.
References
- Genetic Home Reference https://ghr.nlm.nih.gov/condition/critical-congenital-heart-disease#inheritance
- Center for Disease Control https://www.cdc.gov/ncbddd/heartdefects/screening.html
- Akl C. Fahed and Georges M. Nemer (2012). Genetic Causes of Syndromic and Non-Syndromic Congenital Heart Disease, Mutations in Human Genetic Disease, Prof. David Cooper (Ed.), InTech, DOI: 10.5772/48477.