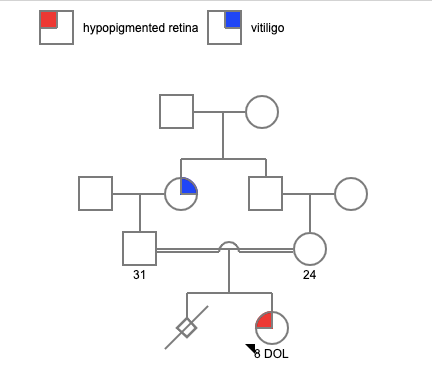
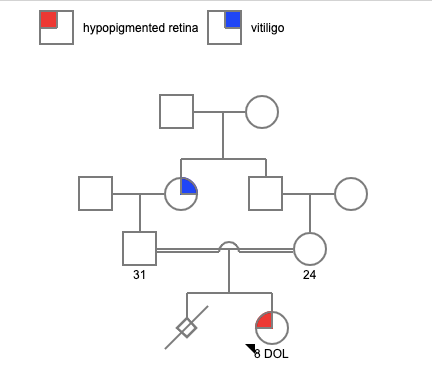
Mr. S, the father of a newborn, presented for a pretest genetic counseling session just 8 days after the birth of his baby girl. This is the first child for this young couple and the excitement for their child soon turned into anxiety after a series of tests were ordered. She was born to consanguineous parents at 34 weeks by LSCS due to low heart beat and polyhydramnios with a birth weight of 1.54 kg and cried 2 mins after birth. Antenatal history was uneventful.
On examination she was found to have blonde hair and a hypopigmented retina. She was suspected of having oculocutaneous albinism (OCA).
The clinician advised undergoing genetic testing, specifically recommending Whole Exome Sequencing (WES). OCA is a group of phenotypically similar genetic disorders derived from errors in melanin synthesis. The most dramatic effects are in the eyes and skin. The skin manifestations are more heterogeneous and appear along with a spectrum of severity depending upon the subtype of OCA. To date, seven types of nonsyndromic albinism (OCA1 to OCA7) have been described. These are all due to isolated genetic mutations whose constellation of signs and symptoms do not manifest so broadly that they can be classified as syndromic. The syndromic albinism such as Hermansky-Pudlak syndrome (HPS) and Chediak-Higashi syndrome (CHS) have the same hallmark lack of dermal and ocular pigment as OCA.
While the WES reports were awaited, the baby girl unfortunately passed away due to respiratory failure. She was reported to have severe hypotonia. After discussion with the doctor and the consent of the parents, a blood sample was provided for DNA storage.
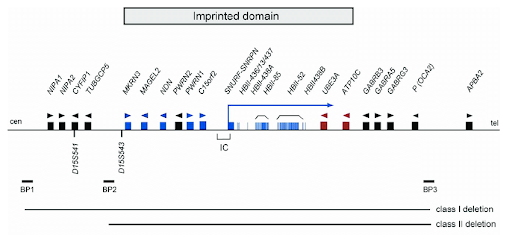
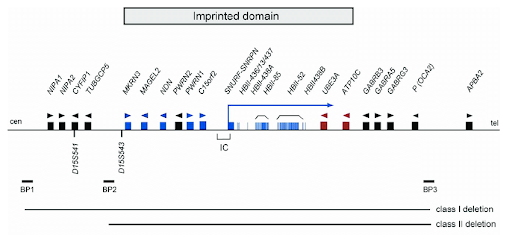
The reports of the Whole Exome Sequencing found a copy number variation in chromosome 15. A 1.75 MB deletion was identified in the 15q region of the chromosome involving genes GABRA5; GABRG3; HERC2; OCA2. OCA2 deletion is associated with Oculocutaneous albinism. This deletion is classified as pathogenic. WES reports identified that there was a deletion in the area very close to the Prader Willi critical region.
While the WES reports were awaited, the baby girl unfortunately passed away due to respiratory failure. She was reported to have severe hypotonia. After discussion with the doctor and the consent of the parents, a blood sample was provided for DNA storage.
The reports of the Whole Exome Sequencing found a copy number variation in chromosome 15. A 1.75 MB deletion was identified in the 15q region of the chromosome involving genes GABRA5; GABRG3; HERC2; OCA2. OCA2 deletion is associated with Oculocutaneous albinism. This deletion is classified as pathogenic. WES reports identified that there was a deletion in the area very close to the Prader Willi critical region.
Follow up testing:
- As the deletion was identified very close to the critical region on PWS and the child clinically was found to have severe hypotonia, we recommended follow up testing by chromosomal microarray to confirm the deletion and identify if the Prader willi region was involved. We used the stored DNA sample for this test. The CMA results confirmed that the child indeed has a pathogenic, heterozygous deletion on chromosome 15 at 15q11.2-q13, involving the Prader-willi/Angelman critical region.
- Methylation studies for the child’s sample is recommended for a confirmation of the Prader willi syndrome.
- Carrier screening and karyotyping in parents have been recommend for further risk assessment for future pregnancies
The impact of genetic counseling
Pretest genetic counseling can help individuals to make informed decisions and anticipate the potential consequences of the results. In this case, the couple was able to prepare for the possible outcomes of the reports, discuss the impact of the diagnosis, treatments, recurrence and causes of the disease. It also allowed them to discuss their emotions and reactions to diagnosis. The post test genetic counseling was greatly impactful in addressing the complexity of the result, requirement for multiple follow up tests, and mainly addressing the grief of losing the child. It was a conundrum for the family, a journey that started with confirmation of a diagnosis however, ended with more questions and dual diagnoses in place. This case also highlighted the barriers to access for mental health as they were unable to receive long term support for grief counseling. Models like telemedicine, providing care in local language, social workers and counselor support in tertiary health care centers can help overcome these barriers.